Quick take
- The biggest wins for canine arthritis usually come from (1) smart nutrition & targeted supplements, (2) gentle movement and rehab, (3) environment tweaks that reduce day-to-day strain.
- PEMF (Pulsed Electromagnetic Field) therapy is a non-drug, non-invasive add-on that can help with pain and mobility and is backed by veterinary studies in dogs with osteoarthritis. (pvj.com.pk, PMC)
- Use several small levers together: weight control, omega-3s/GLM, hydrotherapy/walk plans, orthopedic bedding, traction—and add PEMF to help calm inflammation and support tissue repair.
Understanding your dog’s arthritis—plain and simple
Osteoarthritis (OA) is the most common chronic pain condition in dogs. Cartilage thins, the joint capsule becomes inflamed, and the brain learns pain patterns that can persist even on “good” days. That’s why a single silver bullet rarely works; your best results come from a multimodal plan that tackles pain, inflammation, mobility and lifestyle at the same time.
Below are three natural remedy pillars you can start right away—followed by a deep dive on PEMF therapy and the science behind it.
Pillar 1: Nutrition & supplement strategy (what goes in shapes how they move)
1) Get to (and hold) a lean body condition
A lean dog is a happier, more mobile dog. Every extra kilogram multiplies the load on hips, elbows and knees—and fat tissue produces inflammatory cytokines that worsen OA pain. Work with your vet to set a target body condition score (BCS 4–5/9) and reduce calories gradually (10–15% to start). Choose high-protein, lower-calorie meals so your dog loses fat—not muscle.
Pro tip: Measure portions with a scale, not a scoop. Add lightly cooked low-starch veggies (green beans, courgette) to increase volume without spiking calories.
2) Omega-3s (EPA/DHA) from fish oil
Marine omega-3s help down-regulate inflammatory pathways that drive joint pain. Clinical dosing often targets ~70–100 mg/kg combined EPA+DHA per day (check label concentrations; ask your vet if your dog has a clotting disorder or is on medication). Expect 4–6 weeks for full effect.
3) Green-lipped mussel (GLM)
GLM provides ETA, EPA/DHA, glycosaminoglycans and antioxidants. Randomized studies in dogs have shown improvements in pain and mobility with high-quality GLM extracts. Look for products that disclose ETA content and are stabilized (lipid oxidation kills the benefit).
4) Curcumin & boswellia (with piperine or phospholipid complex)
These botanicals have COX/LOX-modulating effects and can complement omega-3s. Choose formulas designed for dogs; avoid human capsules with xylitol or other unsafe excipients.
5) Collagen peptides & undenatured type II collagen (UC-II®)
Hydrolyzed collagen feeds cartilage building blocks; UC-II may tamp down immune over-response to joint cartilage. Some dogs respond best to a combo of marine omega-3 + GLM + collagen.
Stack idea:
- Morning: Fish oil + GLM
- Evening: Collagen peptide + curcumin/boswellia
- Re-check progress at 6–8 weeks and tweak.
Pillar 2: Movement, rehab, and bodywork (motion is lotion—done the right way)
1) Daily “joint-smart” walks
Many arthritic dogs over-do weekend adventures and under-move on weekdays. Swap “boom-and-bust” for two to three short, even walks (10–20 minutes each on flat ground), keeping a loose lead and sniff breaks. Add 5% distance per week if your dog finishes relaxed.
2) Hydrotherapy or warm-water swimming
Buoyancy reduces joint load while water provides resistance to build muscle safely. A canine hydrotherapist can tailor intervals and monitor gait symmetry.
3) Physio exercises at home
- Weight shifts (standing, gentle side-to-side)
- Cookie stretches (nose to shoulder/hip)
- Cavaletti rails (low obstacles promote proprioception)
- Sit-to-stand sets (start with 3–5 reps)
Two short sessions (3–5 minutes) beat one long one.
4) Massage & myofascial release
Chronic OA drives compensatory muscle tightness. Light effleurage strokes toward the heart, trigger-point holds (5–8 seconds) and heat packs (never hot) can drop pain levels before walks.
5) Non-invasive modalities
PEMF (deep dive below), low-level laser therapy (LLLT) and acupuncture are all widely used by veterinary pain/rehab clinics as drug-sparing tools.
Pillar 3: Home & lifestyle tweaks (comfort is treatment)
- Orthopedic memory-foam bed: 3–4 inch base, sized so your dog can stretch; place away from drafts.
- Traction: Non-slip runners, toe grips, or paw wax prevent splits and falls that aggravate joints.
- Ramps: Bed, sofa, and car ramps save thousands of jump-impacts per year.
- Heat before, cool after: Warmth loosens tissue pre-walk; cool packs reduce post-walk inflammation.
- Nail length & paw care: Long nails change joint angles and strain elbows/hips; keep nails short and rounded.
- Pacing & predictability: Consistent routines reduce over-excitement bursts and “zoomie” setbacks.
Why PEMF belongs in your plan

Pulsed Electromagnetic Field (PEMF) therapy delivers time-varying magnetic fields that induce tiny currents in tissues. In osteoarthritis, those gentle currents can help:
- Reduce inflammatory mediators and edema
- Improve microcirculation and oxygenation
- Support chondrocyte metabolism and mitochondrial ATP
- Modulate pain signaling (central and peripheral)
What the peer-reviewed dog studies say
- Pinna et al., Pakistan Veterinary Journal (2013) – Clinical study in dogs with osteoarthritis showed statistically significant reductions in pain and improved function during a PEMF treatment course. Importantly, benefits persisted longer than the pharmacologic comparison after therapy ended. (pvj.com.pk)
- Sprunks et al., 2024 (Randomized, double-blinded, placebo-controlled) – 60 dogs with OA completed a 14-day course of pulsed short-wave electromagnetic field therapy. The treatment group showed improvements in quality-of-life behaviors associated with discomfort and better passive range of motion, compared with sham. (PMC)
- Leung et al., 2024 (Randomized, controlled, double-blinded, cross-over) – Eight dogs with hip OA received one PEMF session vs. sham in a cross-over design. The paper evaluated immediate changes in pain/lameness; although a single session is a tough test, randomized veterinary PEMF trials like this strengthen the evidence base and inform parameters used clinically. (PMC, BioMed Central, PubMed)
There are also veterinary reviews and guidance pieces noting reductions in clinical OA signs after multi-session PEMF protocols, and summarizing mixed but encouraging evidence (differences often come down to frequency, intensity, coil placement, and session dose). (ScienceDirect, Wiley Online Library, Vca)
What this means for your dog
- PEMF isn’t a drug and typically has very few side-effects when used correctly.
- It fits beautifully alongside weight loss, supplements, movement therapy, and comfort upgrades.
- Many owners report better ease-of-movement in the morning, more willingness to walk, and less “after-walk stiffness.”
A step-by-step PEMF plan you can discuss with your vet
Always check with your veterinarian first—especially if your dog has an implanted electronic device, is epileptic, or has an undiagnosed mass.
Goal: reduce pain behaviors, improve mobility and quality of life.
Weeks 1–2 (gentle start)
- Frequency: 10 Hz (relaxation/anti-inflammatory)
- Session length: 10 minutes, twice daily on the most painful joint or over the spine segment that serves the limb
- Intensity: Low–moderate (you’re aiming for comfort, not maximum power)
Weeks 3–4 (build dose)
- Alternate 10 Hz and 25–35 Hz sessions (some canine protocols use 33 Hz for joint tissue).
- Duration: 15 minutes, twice daily
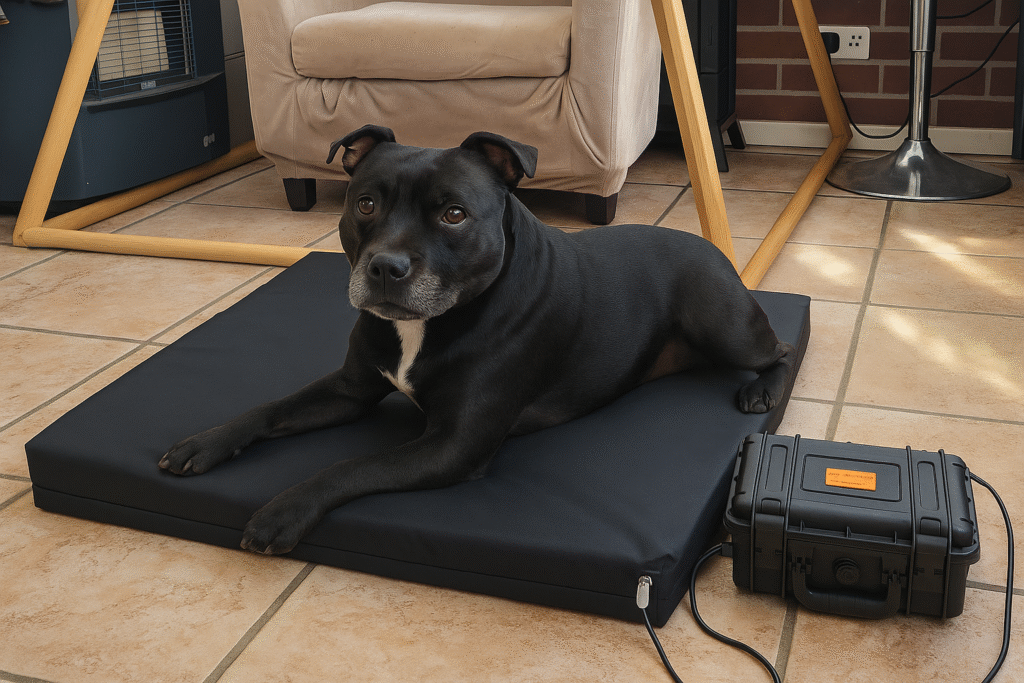
- If you’re using a mat as well, add one whole-body session in the evening (8–10 Hz for 15–20 minutes) to support sleep and systemic inflammation.
Weeks 5–8 (maintenance & evaluate)
- Frequency mix: 10 Hz on “sore” days, 33 Hz on “stiff” days; add the mat 3–5 nights/week.
- Duration: 15–20 minutes once daily, with a second short “top-up” on flare days.
- Keep a simple log: ease of rising, stairs, after-walk stiffness (0–10), and any changes in play.
Placement tips
- For hips: one coil each side of the pelvis, or a flexible coil around the thigh.
- For elbows/shoulders: coil lateral to the joint; avoid direct pressure on bony points.
- For spine-linked lameness: place over the cervico-thoracic or lumbosacral area that activates the limb (some trials positioned the device near the cervico-thoracic region). (PMC)
When to expect changes
- Some dogs relax during or after sessions; meaningful mobility gains usually appear within 2–4 weeks of consistent use. Keep everything else (walks, diet) steady so you can see the PEMF effect clearly.
Complementary natural tools that stack well with PEMF
- GLM + omega-3s: PEMF reduces inflammatory signaling; omega-3s help keep the fire out.
- Hydrotherapy: PEMF reduces pain enough to allow gentler, better-quality movement in water sessions.
- Acupuncture: Useful where central sensitization (learned pain) is a big piece of the puzzle.
- Joint-friendly flooring + ramps: Keeps the gains you earn from PEMF and rehab from being erased by slips and jumps.
Troubleshooting: if progress stalls
- Re-check weight: Even a small reduction in BCS can unmask improvements.
- Move to twice-daily sessions for 10–14 days, then taper.
- Change the target: If you’ve been treating the hip, try the lumbosacral spine or gluteal trigger points as your primary coil location for a week.
- Ask your vet to layer options: NSAIDs or gabapentin for a short course can break flare cycles while PEMF and rehab build momentum.
- Assess sleep & stress: Poor sleep = higher pain scores. Night PEMF mat sessions often help.
Safety, side-effects and common-sense rules
- Don’t use PEMF over active cancers, untreated infections, or fresh surgical sites unless your vet approves a protocol.
- Avoid use with implanted electronic devices (pacemakers, spinal stimulators).
- Start low; if your dog seems restless during sessions, lower intensity, reduce duration, or increase distance from the joint.
- Many dogs enjoy PEMF sessions—watch for soft yawns, sighs, and relaxed posture as your green lights.

How to choose a PEMF option for dogs
- Coil size & flexibility: Elbows and hips need different geometry. Flexible or multiple coils make placement easier.
- Frequency control: Look for low-frequency options (5–50 Hz) and simple presets.
- Intensity range: Enough output to treat deep joints—but also the ability to dial down for comfort.
- Build & support: Durable cables, pet-safe materials, responsive support, and a clear return policy.
- Portability: Battery or USB power is convenient for multi-room homes and travel.
Realistic results you can expect
- First 1–2 weeks: calmer rest, easier transitions from lying to standing, less paw-licking around sore joints.
- Weeks 3–6: longer comfortable walk distances, smoother stairs, more willingness to play.
- Ongoing: fewer “bad days,” lower reliance on breakthrough meds, better mood and engagement.
Remember: no single therapy “cures” OA. You’re raising quality of life by stacking safe wins and keeping them consistent.
Evidence snapshot (in dogs)
- PEMF clinical study—dogs with OA: Reduced pain and improved function; effects persisted after treatment vs. control. (pvj.com.pk)
- Randomized, double-blind, placebo-controlled (14 days, 60 dogs): Improved behaviors/QoL and passive range of motion vs. sham; device near cervico-thoracic region. (PMC)
- Randomized, controlled, double-blind, cross-over (single session, hip OA): Immediate-effect investigation informing parameters and tolerability. (PMC)
- Reviews & summaries: Veterinary overviews note reductions in OA signs after multi-session PEMF, with variability tied to protocol differences—underscoring the value of device control over frequency/intensity and consistent dosing. (ScienceDirect, Wiley Online Library, Vca)
Putting it all together (your 6-week plan)
- Trim and nourish
- Set a lean-weight target; weigh meals.
- Start omega-3 + GLM (and optionally collagen + curcumin/boswellia).
- Move smart
- Two short, even walks daily; add 3–5 minutes of physio drills.
- One hydro session/week if available.
- Make home dog-friendly
- Orthopedic bed, non-slip paths, ramps, short nails.
- Add PEMF—daily
- Weeks 1–2: 10 Hz, 10 minutes, twice daily.
- Weeks 3–4: alternate 10 Hz and 33 Hz, 15 minutes, twice daily.
- Weeks 5–6: once daily 15–20 minutes; mat sessions at night 3–5×/week.
- Recheck
- Keep a simple mobility log and video your dog before starting and at week 6; share with your vet to adjust the plan.
FAQs
Is PEMF safe for older dogs?
Generally, yes—when used as directed. It’s non-thermal and non-invasive. Always check with your vet if your dog has implants, seizures, bleeding disorders, or active tumors.
Can PEMF replace medications?
Think of it as drug-sparing, not a replacement. Many dogs need less medication over time, but decisions about NSAIDs, gabapentin, or joint injections should be made with your veterinarian.
How long do results last?
PEMF isn’t a one-off cure; arthritis is chronic. Expect to keep short, regular sessions in your routine, just like daily walks and joint-smart nutrition.
Will my dog feel the pulses?
Most don’t feel a thing—many doze off during sessions. Restlessness means you should lower intensity or shorten the session.
The bottom line
For dogs with arthritis, natural remedies work best together: keep your dog lean, feed the joints (omega-3s/GLM/collagen), move smartly, and make home comfortable. Then add PEMF to calm inflammation and encourage easier movement. The veterinary literature—including randomized, blinded dog studies—supports PEMF as a useful adjunct for pain and mobility when used in consistent, multi-session protocols. (pvj.com.pk, PMC)
If you want help tailoring a dog-specific PEMF schedule (by weight, joint, and home device type), tell me your dog’s age, weight, main sore joints, and the PEMF model you’re using—I’ll map out a clean, week-by-week plan you can review with your vet.